Marvellous Medical Materials: Stainless Steel - Part Two
01 December 2017

In this series of blog posts, Sarah Wilkes (Wellcome Trust Research Fellow at the Institute) gets over-excited about the ways that materials like silicone rubber and silver impact on our health and wellbeing. This post is the second in a two-parter that focuses on steel. My previous blog post focused on the gradual historical domination of stainless steel in surgical tools and in vivo applications, and discussed the health risks and rewards of its use for a variety of actors, including the patient undergoing hip replacement and the welder. This second blog post focuses on the use of stainless steel in the wider hospital environment and its role in infection control.
Stainless steel has health impacts beyond its use in surgical instruments, implantable devices and the occupational hazards of its manufacture. In the face of recent concerns about antimicrobial resistance and hospital acquired infections (HAIs), there has been increased interest in the ways in which materials and surfaces allow for or encourage the growth of particular bacteria such as Methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa and Escherichia coli (E. coli). As a result of this concern with infection-control, stainless and polymer-coated steels seem to have become one of the most dominant materials used in hospital material culture and built environment in the UK, alongside a multitude of hard plastics. Organic materials and soft furnishings (e.g. woods and textiles) are being actively deselected by some NHS Trusts.
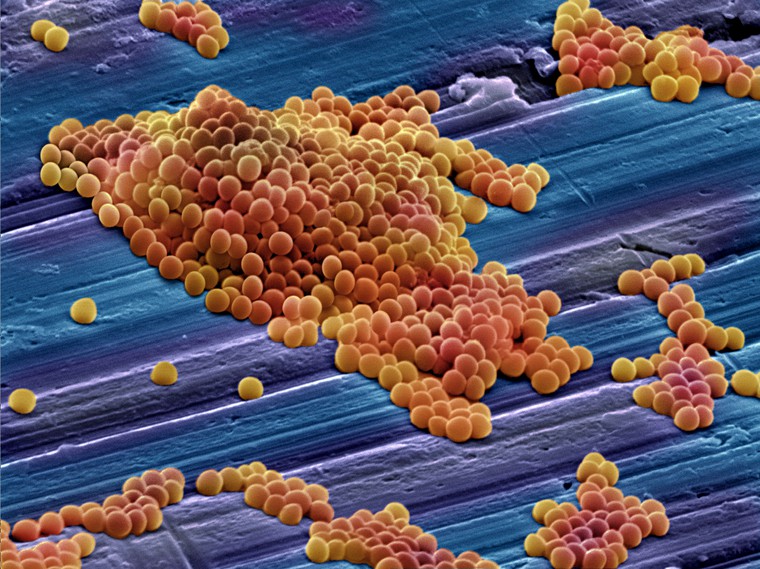
Image credit: 'MRSA' by Annie Cavanagh. Source: Wellcome Images.
However, the mechanisms by which bacteria adhere to and persist on different materials in a hospital environment are very complex, and still only partially understood. A great deal of work has been done to examine how surface roughness and topography, hydrophobicity, surface charge, stiffness and porosity[1] impact on bacterial adhesion, growth and persistence. However, most of these are lab-based studies of new and pristine surfaces, with only a handful simulating the wear and repeated cleaning of surfaces that materials in hospitals undergo (Verran et al. 2001; Carpentier et al. 1993).There’s also a great deal of work being done to develop future materials for infection control, with new biocidal, anti-fouling and anti-adhesive surfaces being synthesized in labs at UCL and further afield (Noimark et al. 2014, Page et al. 2008). In the shorter term though, what’s missing is advice to guide healthcare designers and architects in selecting from the palette of materials that’s currently available.
I have been trying to remedy that through a three-year Wellcome Trust research fellowship. The overall aim of the project (called Materials Anxieties for short) is to better understand how materials used in small healthcare products (such as prosthetics & orthotics, hospital architectural hardware & furniture) affect patient and clinician experiences of health and wellbeing in positive and negative ways. The ultimate goal is to feed the project results back to materials developers, healthcare designers and architects with the aim of encouraging the development and selection of materials that better meet the needs of patients and clinicians.
One obvious way in which materials and surfaces affect health is through their interactions with microorganisms and impact on infection control. I have therefore been surveying London hospitals to put together a database of the materials most-used in beds, overbed tables and other high-touch surfaces that are known to harbour infections; doing in-situ materials analysis to look at the roughness and surface topography of materials that have been in everyday use in a hospital environment for several years; and conducting research with healthcare designers and architects to understand how they currently select materials for hospital material culture. I hope to bring all of this together to develop some materials selection guidance for healthcare architects and designers later on in the project. Watch this space…
So far, interest in the ways in which materials impact on patient health has primarily focused on their technical properties, and there is also almost nothing written about the human impact of these material choices beyond their immediate physiological effects[2]. Stainless steel is often selected for healthcare applications in preference to other metals, polymers and organic materials because of its perceived superior technical properties: its low cost, relative durability, comparatively smooth finish, resistance to standard cleaners, and relative ease of cleaning. Its dominance is not just down to these technical properties however, but also its sensory and aesthetic properties and cultural associations: like its “clean appearance” (Bergman et al. 2014). As part of this research project I am also interested in understanding how the sensory, aesthetic, affective and cultural affordances of materials (as well as their physical or functional properties) influence peoples' experiences of different healthcare products and environments.
[1] See Harris & Martin 1987, Flint et al. 2000, Katsikogianni & Missirlis 2004, Katainen et al. 2006, Anselme et al. 2010, Ribiero et al. 2012, Rzhepishevska et al. 2013, Song and Ren 2014 and Song et al. 2015 for further reading.
[2] Whilst the therapeutic effects of nature, visual art, lighting, colour and design have been observed by health geographers and architects (Ulrich 2001; Tse et al. 2002; Dalke at al. 2006; Caspari et al. 2006 and Schifferstein et al. 2007) no attention has yet been paid to materials.
References
Anselme, K., Davidson, P., Popa, A. M., Giazzon, M., Liley, M., & Ploux, L. (2010). The interaction of cells and bacteria with surfaces structured at the nanometre scale. Acta biomaterialia, 6(10), 3824-3846.
Bergman, M., Rosén, B. G., Eriksson, L., & Anderberg, C. (2014, June). Surface Design Methodology-The Cleanability Investigation. In KEER2014. Proceedings of the 5th Kanesi Engineering and Emotion Research; International Conference; Linköping; Sweden; June 11-13 (No. 100, pp. 705-722). Linköping University Electronic Press
Carpentier, B., & Cerf, O. (1993). Biofilms and their consequences, with particular reference to hygiene in the food industry. Journal of Applied Microbiology, 75(6), 499-511
Caspari , S., Eriksson, K., & Nåden, D. (2006). The Aesthetic Dimension in Hospitals—An Investigation Into Strategic Plans. International Journal of Nursing Studies 43(7): 851-859.
Dalke, H., Little, J., Niemann, E., Camgoz, N., Steadman, G., Hill, S., & Stott, L. (2006). Colour and Lighting in Hospital Design. Optics & Laser Technology 38(4): 343-365.
Flint, S. H., Brooks, J. D., & Bremer, P. J. (2000). Properties of the stainless steel substrate, influencing the adhesion of thermo-resistant streptococci. Journal of Food Engineering, 43(4), 235-242
Harris, J. M., & Martin, L. F. (1987). An in vitro study of the properties influencing Staphylococcus epidermidis adhesion to prosthetic vascular graft materials. Annals of surgery, 206(5), 612.
Katainen, J., Paajanen, M., Ahtola, E., Pore, V., & Lahtinen, J. (2006). Adhesion as an interplay between particle size and surface roughness. Journal of Colloid and Interface Science, 304(2), 524-529
Katsikogianni, M., & Missirlis, Y. F. (2004). Concise review of mechanisms of bacterial adhesion to biomaterials and of techniques used in estimating bacteria-material interactions. Eur Cell Mater, 8(3).
Noimark, S., Allan, E., & Parkin, I. P. (2014). Light-activated antimicrobial surfaces with enhanced efficacy induced by a dark-activated mechanism. Chemical Science, 5(6), 2216-2223.
Page, K., Wilson, M., & Parkin, I. P. (2009). Antimicrobial surfaces and their potential in reducing the role of the inanimate environment in the incidence of hospital-acquired infections. Journal of Materials Chemistry, 19(23), 3819-3831.
Ribeiro, M., Monteiro, F. J., & Ferraz, M. P. (2012). Infection of orthopedic implants with emphasis on bacterial adhesion process and techniques used in studying bacterial-material interactions. Biomatter, 2(4), 176-194
Rzhepishevska, O., Hakobyan, S., Ruhal, R., Gautrot, J., Barbero, D., & Ramstedt, M. (2013). The surface charge of anti-bacterial coatings alters motility and biofilm architecture. Biomaterials Science, 1(6), 589-602
Schifferstein, H. N. & Desmet, P. M. (2007). The Effects of Sensory Impairments on Product Experience and Personal Well-Being. Ergonomics 50(12): 2026-2048.
Song, F., & Ren, D. (2014). Stiffness of cross-linked poly (dimethylsiloxane) affects bacterial adhesion and antibiotic susceptibility of attached cells. Langmuir, 30(34), 10354-10362
Song, F., Koo, H., & Ren, D. (2015). Effects of material properties on bacterial adhesion and biofilm formation. Journal of dental research, 94(8), 1027-1034
Tse, M. M., Ng, J. K., Chung, J.W., Wong, T. K. (2002). The Effect of Visual Stimuli on Pain Threshold and Tolerance. J. Clin Nurs 11: 462–9.
Ulrich, R. (2001). Effects of Healthcare Environmental Design on Medical Outcomes. In Design and Health: Proceedings of the Second International Conference on Health and Design. Stockholm, Sweden
Verran, J., Boyd, R. D., Hall, K., & West, R. H. (2001). Microbiological and chemical analyses of stainless steel and ceramics subjected to repeated soiling and cleaning treatments. Journal of food protection, 64(9), 1377-1387.